Article Highlights
-
Researchers developed a 3D airway-on-a-chip that mimics living lung tissues.
-
Organs-on-chips are a way to screen drugs for activity against SARS-CoV-2.
-
Amodiaquine, a malaria drug, showed antiviral activity in the airway chip and is being tested in humans.
What’s happening in the lab of Donald Ingber, M.D., Ph.D., sounds like something from the distant future.
Ingber and his team at the Wyss Institute for Biologically Inspired Engineering at Harvard University are creating organs-on-chips — tiny, complex 3D models of living human organs. Their work has been supported by the National Center for Clinical and Translational Sciences (NCATS) for years. But now, with additional funding from NCATS and other sources, they’re experimenting with an airway chip that could help in the search for new treatments for COVID-19.
“Current methods to screen drugs for effectiveness before they are given to humans are not ideal,” said Danilo A. Tagle, Ph.D., Associate Director of Special Initiatives at NCATS, which oversees the Tissue Chip for Drug Screening Program. “Organ chips mimic the structure and function of human organs. This means that they may be able to model diseases such as COVID-19 and predict antiviral activity of drugs more accurately and quickly than animal studies can.”
Ingber is the founding director of the Wyss Institute and a professor at Harvard University’s Schools of Medicine and Engineering and Boston Children’s Hospital. He spoke with us about developing the airway chip and using the technology as a rapid method for identifying potential treatments for viral infections, such as influenza and COVID-19.

Donald Ingber has been at the forefront of organ-on-a-chip technology since 2010. The miniature devices mimic the structure and function of human organs and may predict drug safety and effectiveness more accurately than animal studies do. Photo courtesy of the Wyss Institute at Harvard University.

Donald Ingber has been at the forefront of organ-on-a-chip technology since 2010. The miniature devices mimic the structure and function of human organs and may predict drug safety and effectiveness more accurately than animal studies do. Photo courtesy of the Wyss Institute at Harvard University.
NIH: Tell us about the organ-on-a-chip technology your team has been working on.
INGBER: Organ chips contain lab-grown human cells like other culture systems, but the cells mature and organize to create the tissue-to-tissue interfaces that make up organs. The chips are like 3D cross-sections of major parts of human organs, and they also mimic the way the organ functions. Yet they are no bigger than a USB drive.1
At the Wyss Institute, we have created more than 15 different organ chips, including a lung airway chip. We’ve been using it to study diseases like asthma, chronic obstructive pulmonary disease, and influenza (flu).1-3
But in response to COVID-19, we’ve gone a step farther with the airway chip.1 Our experiments are providing valuable information about how pandemic viruses, such as SARS-CoV-2, invade lung cells and how the body’s immune system reacts.

Accelerating Drug Testing with the Airway Chip
Ingber’s team is using the technology to screen drugs for use against COVID-19.
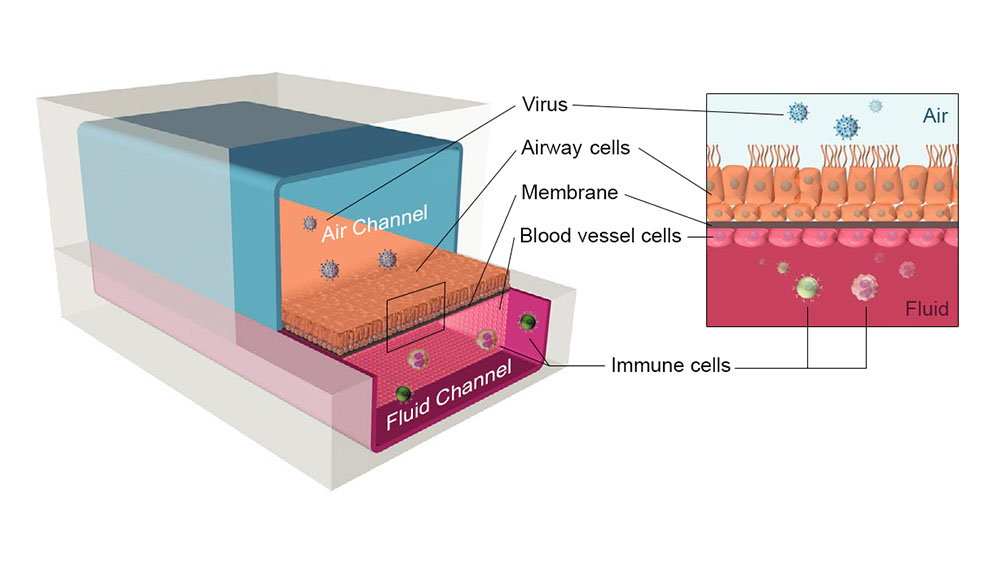
The airway chip consists of layers of lung and blood vessel cells that function much as they do in actual human lungs. Fluid and air flow through the channels on either side of a porous membrane. Researchers have infected the chips with influenza viruses and SARS-CoV-2 pseudovirus. They can then observe reactions of the lung tissue and immune cells. Image courtesy of the Wyss Institute at Harvard University.
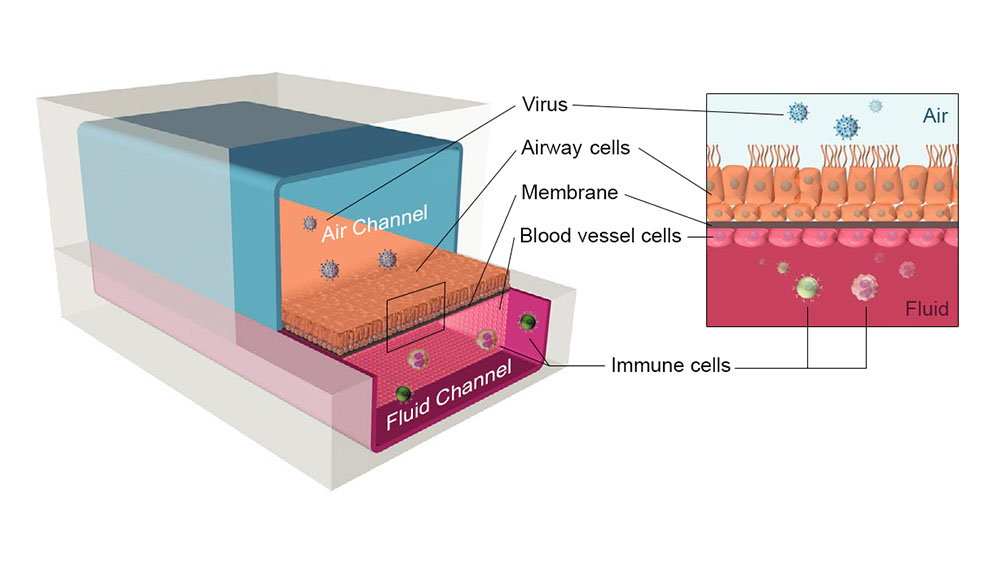
The airway chip consists of layers of lung and blood vessel cells that function much as they do in actual human lungs. Fluid and air flow through the channels on either side of a porous membrane. Researchers have infected the chips with influenza viruses and SARS-CoV-2 pseudovirus. They can then observe reactions of the lung tissue and immune cells. Image courtesy of the Wyss Institute at Harvard University.
NIH: How do you construct airway chips?
INGBER: The airway chips are made of a clear, flexible polymer. They contain two parallel microchannels the width of a pencil lead. A porous membrane separates the microchannels. One of the tiny channels is for fluid, and the opposite one is for air. We take primary human cells — cells from samples of airway tissue — and apply the cells to the membrane. The cells multiply, and after two or three weeks, they mature into the specialized cell types of the lung airway — just as they exist in a human lung. Lung cells grow on the air side of the membrane, and cells that line blood vessels grow on the other, with a pump moving culture medium through the fluid channel.
Some of the lung cells in the airway chip actually create mucus and even grow cilia, tiny hairlike structures that move mucus and help protect the body from infection.
NIH: How can the airway chip help us learn about COVID-19?
INGBER: As we first showed with influenza virus, the power of the airway chip is that it allows us to study viral infection and to observe immune responses. In our studies, we used a pseudovirus — a harmless virus that enters cells the same way that SARS-CoV-2 does. The pseudovirus allows us to safely study the initial stages of infection and viral entry into lung cells.
Some severe COVID-19 symptoms aren’t caused by the virus itself but rather by an overactive inflammatory response. With the airway chip, we can study the fluid exiting the system — much like taking a blood sample — to learn about cell responses to infection. We can run experiments to perhaps identify ways to prevent or treat dangerous inflammation.
“Organ chips mimic the structure and function of human organs. This means that they may be able to model diseases such as COVID-19 and predict antiviral activity of drugs more accurately and quickly than animal studies can.” —Danilo A. Tagle, Ph.D.
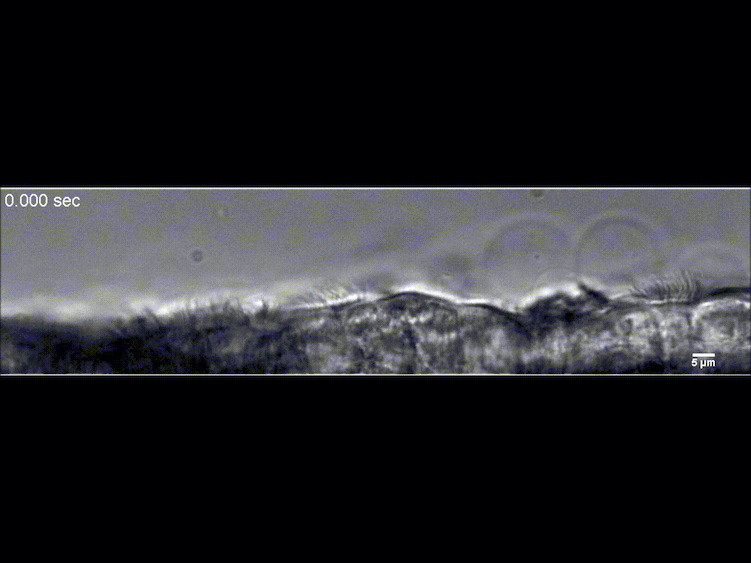
The sweeping motion of cilia on lung cells in the airway chip. In the human lung, cilia help remove invading organisms from the airway. Video courtesy of the Wyss Institute at Harvard University.
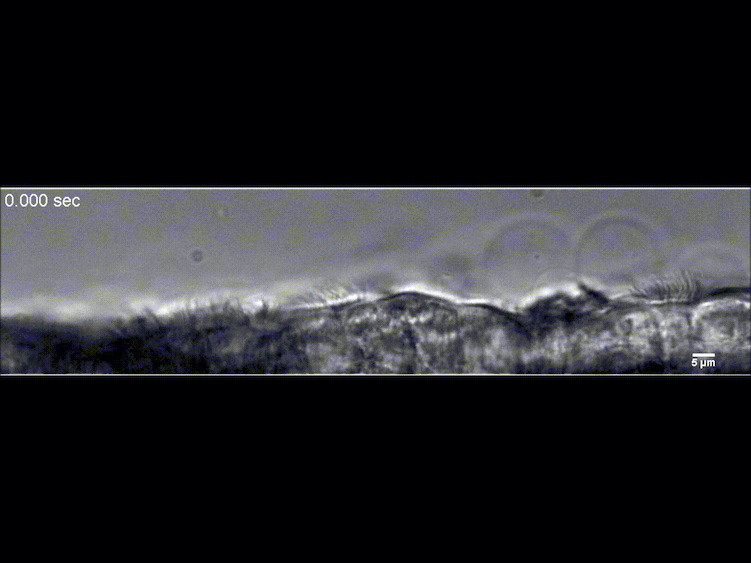
The sweeping motion of cilia on lung cells in the airway chip. In the human lung, cilia help remove invading organisms from the airway. Video courtesy of the Wyss Institute at Harvard University.
NIH: What is the role of the airway chip in developing treatments for COVID-19?
INGBER: There are many ways the chip can be used. We’re using the airway chip to screen drugs as potential treatments for COVID-19. We first focused on testing drugs that the FDA has already approved for treating other diseases. Because the airway chip has a fluid channel and an air channel, we’re able to study drugs given by injection or breathed into the airway (like with an inhaler). Our research may identify drugs that could keep the virus from infecting cells or calm overactive immune responses.
We’re also using the airway chip to identify viral variants that can evolve when viruses are exposed to antiviral drugs.
NIH: What’s an example of using the airway chip to screen possible treatments for COVID-19?
INGBER: With funding from NIH and the Defense Advanced Research Projects Agency, we identified eight compounds, including some malaria drugs, that prevented the SARS-CoV-2 pseudovirus from invading cells grown in petri dishes. However, these simple 2D culture systems often don’t mimic what happens in the human body.
To get a better idea of how the drugs might perform in human disease, we tested the same compounds in airway chips we infected with the SARS-CoV-2 pseudovirus. When we tested chloroquine and hydroxychloroquine, we found that neither drug stopped the virus, and most of the other drugs did not work either. However, amodiaquine — an inexpensive malaria drug widely used in Africa — significantly reduced pseudovirus infection in the airway chips. In hamster experiments, amodiaquine reduced infections and prevented spread of infectious SARS-CoV-2 as well. The drug is now being tested in human studies as a possible COVID-19 treatment.2
NIH: What’s next for the airway chip?
INGBER: With additional NIH support, we are using the chip to develop broad-acting medicines that may be able to prevent infections caused by many different coronaviruses and influenza viruses.
In addition, we are studying inflammatory responses to viral infections within the alveoli (air sacs of the lungs) using an alveolus chip that mimics breathing motions and immune effects. This work has identified potential molecular targets in cells that drugs can bind to avert severe immune responses, including cytokine storms that can damage organs.
To take our COVID-19 experiments to the next level, we’d like to study the infectious form of SARS-CoV-2 in the airway chip. But that type of work requires the more protective environment of a Biosafety Level 3 lab. We are beginning to do this research through collaboration.
NIH has provided us with long-term support that has advanced organ chip research. There’s great interest in this technology, because it could cut the time and cost of developing new drugs and vaccines. When it comes to public health emergencies like the COVID-19 pandemic, organs-on-chips could save lives.
Sources
-
Benam, K. H., Villenave, R., Lucchesi, C., Varone, A., Hubeau, C., Lee, H. H., Alves, S. E., Salmon, M., Ferrante, T. C., Weaver, J. C., Bahinski, A., Hamilton, G. A., & Ingber, D. E. (2016). Small airway-on-a-chip enables analysis of human lung inflammation and drug responses in vitro. Nature Methods, 13(2), 151–157. https://doi.org/10.1038/nmeth.3697
-
Si, L., Bai, H., Rodas, M., Cao, W., Oh, C. Y., Jiang, A., Moller, R., Hoagland, D., Oishi, K., Horiuchi, S., Uhl, S., Blanco-Melo, D., Albrecht, R. A., Liu, W.-C., Jordan, T., Nilsson-Payant, B. E., Golynker, I., Frere, J., Logue, J., Haupt, R.,. . .Ingber, D. E. (2021). A human-airway-on-a-chip for the rapid identification of candidate antiviral therapeutics and prophylactics. Nature Biomedical Engineering. Advance online publication. https://doi.org/10.1038/s41551-021-00718-9
-
Benam, K. H., Novak, R., Nawroth, J., Hirano-Kobayashi, M., Ferrante, T. C., Choe, Y., Prantil-Baun, R., Weaver, J. C., Bahinski, A., Parker, K. K., & Ingber, D. E. (2016). Matched-comparative modeling of normal and diseased human airway responses using a microengineered breathing lung chip. Cell Systems, 3(5), 456–466.e4. https://doi.org/10.1016/j.cels.2016.10.003
 An official website of the United States government
An official website of the United States government


