Article Highlights
-
Children are often excluded from clinical trials of new medicines.
-
NIH is funding the POP02 study to understand how medicines work in children.
-
The study has expanded its scope to include children with COVID-19.
Shacarla “Carlie” Bellamy, age 15, is used to being in the hospital. She has sickle cell disease, in which her blood cells can sometimes become sickle-shaped and cause extreme pain. When she was younger, this would put her in the hospital about three times a year, often for 10 days at a time. As she gets older, her hospital stays have gotten more frequent. “It’s not fun,” she said. But she enjoys joking and chatting with the doctors and nurses, and her friends love to visit — or they did before the COVID-19 pandemic.
On a day early in January 2021, Carlie’s mom, Latisha, knew that it was time to go to the hospital again. “I can tell a certain way she looks in her eyes,” she said. “I can tell she’s really not feeling well, and her pain isn’t being controlled at home.” Latisha drove them 30 miles to the Duke University Hospital in Durham, North Carolina.
Carlie had a little trouble breathing and a headache, but they assumed it was just pneumonia again — a frequent complication of sickle cell disease. Both Latisha and Carlie had been sick and tested positive for COVID-19 in April 2020, so it was a surprise when a test came back positive in the emergency room. “I’m shocked,” Latisha said, remembering. “I’m thinking, at the same time, ‘Oh, God, don’t let her get worse.’”
While she was in the hospital, Carlie became one of about 400 young people up to age 20 who have enrolled in the Pharmacokinetics, Pharmacodynamics, and Safety Profile of Understudied Drugs Administered to Children Per Standard of Care (POP02) study. POP02 is part of the Pediatric Trials Network, a network funded by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD). By joining the study, Carlie is helping researchers understand how COVID-19 affects children and adolescents.
“We’re in the middle of a public health crisis, and we need to unify all of our efforts to combat this. It means everything that there are so many willing families and patients just like Shacarla who, without any hesitation, are willing to assist in this fight with us.” —Chi Hornik

Carlie’s older sister, Ciaquoia, draws pictures and texts them to her sister in the hospital.

Carlie’s older sister, Ciaquoia, draws pictures and texts them to her sister in the hospital.
Modifying a study for COVID-19
POP02’s original purpose was to understand how medicines affect children and teens, who are often not included in the clinical trials that determine whether a medicine is safe and effective. This exclusion means doctors may not have the data to help guide their decisions.
When the pandemic hit in 2020, the study’s leader, Chi Hornik, realized that POP02 could help. As a clinician and researcher at Duke, she works primarily with children and adolescents in the intensive care unit, which includes some patients who get very sick with COVID-19. In March 2020, she and her colleagues expanded the list of medicines being examined in POP02 to include the treatments being used for children and adolescents with COVID-19. Last summer, Hornik and her colleagues modified the protocol again to include people who had COVID-19 but did not need to be treated for it or who came to the hospital with multisystem inflammatory syndrome in children (MIS-C), a rare but serious complication of COVID-19.
“We’re in the middle of a public health crisis, and we need to unify all of our efforts to combat this,” Hornik said. “It means everything that there are so many willing families and patients just like Shacarla who, without any hesitation, are willing to assist in this fight with us.”
Enrolling in the hospital
Carlie did not develop severe COVID-19 but stayed in the hospital for her usual sickle cell treatments, including pain medicine and blood transfusions. She also received a medicine to prevent blood clotting — one of the medicines in the POP02 list.
After Carlie had been in the hospital for about a week, Hornik was checking Duke’s medical records system to see whether any patients might be eligible to enroll in her study. Carlie’s record came up, and Hornik stopped by to chat.
Carlie wasn’t feeling well when Hornik got there. “I asked her if it was okay for me to talk to her, about this opportunity to participate in this trial to help others just like her, and she just completely perked up,” Hornik said.
Hornik explained the study and what Carlie would have to do to participate. The study does not require any new samples from children and teens who enroll. Instead, the researchers use the bloodwork that is done as part of the patient’s regular health care. They look at how the body is responding to treatments and may also do genetic testing. Participants also give permission for the researchers to follow along with their treatment through their medical records, which give a sense of how well the medications worked.
Carlie gave her permission, but because she is a minor, her mother also had to agree. Carlie called Latisha to tell her to say yes. “I remember I was kind of bubbly, excited,” Carlie said. “I thought it was really a super cool thing, that I’d be helping out. I was on board with it.” She is the only person she knows with sickle cell disease and is excited about the idea that she could help other young people with sickle cell disease who also get COVID-19.

Learn more about this study from the Pediatric Trials Network
The Pediatric Trials Network conducts studies on a wide range of diseases in children and adolescents, including COVID-19.
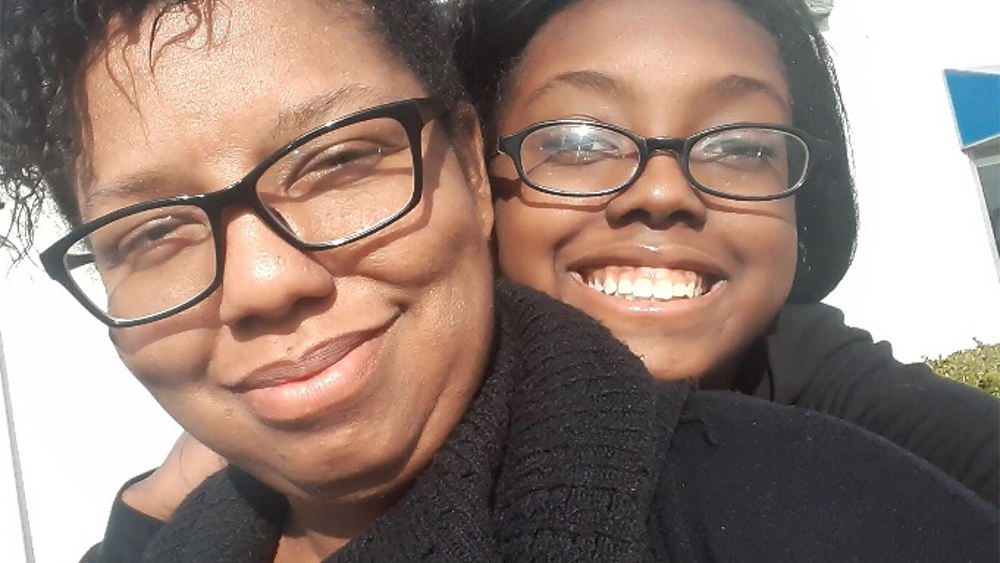
Latisha Bellamy (L) and her daughter Carlie (R).
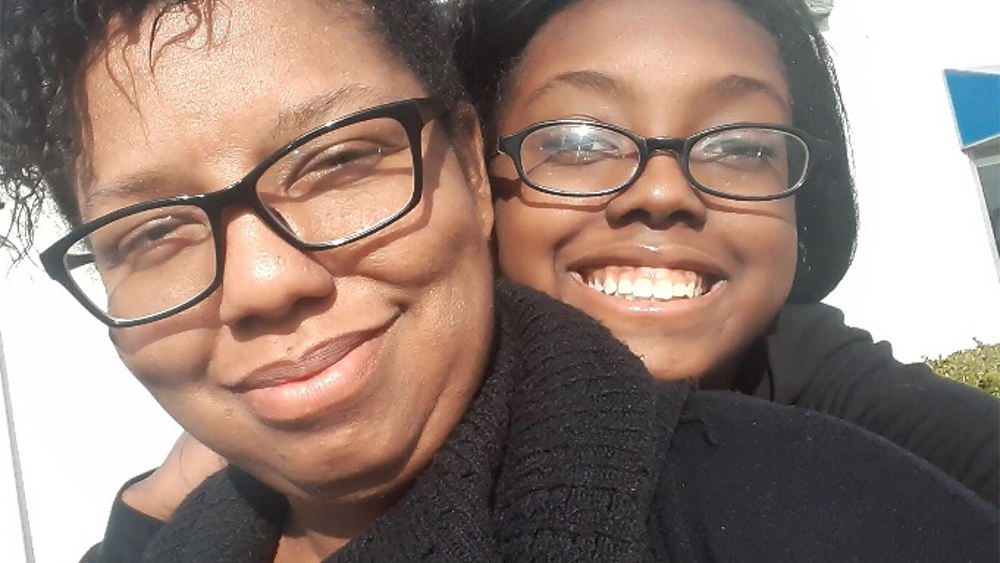
Latisha Bellamy (L) and her daughter Carlie (R).
Studying the effects of COVID-19 on child and adolescent health
Carlie’s experience will help Hornik and her colleagues understand what is going on in the body when a young person has COVID-19 — and how the person’s genetics and other conditions affect the course of the disease. While Carlie did not seem to be seriously ill with COVID-19 when she was in the hospital in January, the disease may have affected her sickle cell symptoms, Hornik said. She and her colleagues are seeing children and adolescents with sickle cell crises that are more severe than usual. The researchers are tracking this to see whether COVID-19 may worsen symptoms in people with sickle cell disease or other chronic diseases, such as diabetes.
POP02 includes about 60 sites in the United States and Canada, and the researchers hope to enroll 5,000 children in the study — including at least 500 with COVID-19. Hornik hopes that the experience of Carlie and other children and teens who, like her, decide to enroll in the study will help shed light on how COVID-19 affects them. “We hope we can better choose drug treatment for children and teens who are affected by COVID.”
 An official website of the United States government
An official website of the United States government


