Article Highlights
-
Researchers are developing smart masks that can detect SARS-CoV-2 in breath and saliva.
-
The masks’ sensors look for enzymes made by coronaviruses.
-
These masks could also be used to detect fungal infections, such as Pneumocystis pneumonia.
In 2023, most people know just what to do when they start feeling sniffly: Head to the pharmacy or their medicine cabinet for a home COVID-19 test, swab, and wait. But what if testing for COVID-19 and other diseases were even simpler and could be conducted more routinely — preventing or stalling outbreaks before they take hold?
Researchers at the University of California, San Diego (UCSD) want it to be that easy. In the summer of 2020, NIH announced its Rapid Acceleration of Diagnostics Radical (RADx-rad) initiative to spark research into nontraditional approaches to COVID-19 testing and surveillance. Jesse Jokerst, Ph.D., and his colleagues proposed developing a mask with a sensor that would collect particles in a person’s breath and saliva all day. The sensor inside the mask could then be activated to see whether the person wearing it had been exposed to SARS-CoV-2, the virus that causes COVID-19, or were infected themselves. With funding from the National Institute of Dental and Craniofacial Research (NIDCR), the research team started putting their idea to the test.
At the time they started thinking about COVID-19 surveillance, masks were on everyone’s minds. Mask guidelines had been in place for a handful of months, and the Centers for Disease Control and Prevention had begun publishing research that showed that masks prevented the spread of the virus. Jokerst, a nanoengineering professor at UCSD, says he and his colleagues started to wonder, “How could we use the face covering not just for protection but also as a type of surveillance?” Disease surveillance — collecting information about a disease — can alert public health officials to developing outbreaks.
While the rise of vaccines and falling numbers of COVID-19 cases have made masks less ubiquitous, masks are still required at many medical facilities and workplaces and remain part of travel and everyday life for many. “A mask with a color-changing sensor could quickly and easily act as a tool to perform surveillance for COVID-19, particularly for groups that may be particularly vulnerable to infectious diseases and may hold more promise for identifying future disease, including fungal diseases and emerging variants of SARS-CoV-2,” Jokerst said.

Jesse Jokerst, Ph.D. Image courtesy of Jesse Jokerst.

Jesse Jokerst, Ph.D. Image courtesy of Jesse Jokerst.
Catching Your Breath
In 2020, the research team began to conduct feasibility studies on whether a mask might be able to capture enough saliva and breath to react to SARS-CoV-2. In a series of experiments, the researchers studied volunteers wearing different types of masks for different periods of time, finding that surgical masks and neck gaiters were good at catching enough saliva and even more effective the longer they were worn. Additionally, the researchers determined that placing a testing strip on the inside of either a mask with ear loops or a neck gaiter might make it possible to capture enough saliva to identify compounds in the breath.
Next, Jokerst and his colleagues started to work on the design of the sensor that would capture saliva. They envisioned a testing strip that could be stuck onto the inside of the mask like a sticker. The testing strip would also have a blister pack of liquid; when they were ready to check their results, the wearer would take off the mask and break the blister pack. The liquid would wash over the testing strip, which would then change color in the presence of SARS-CoV-2.
The researchers tested this strategy by using a testing strip and liquid that would react to amylase, an enzyme in everyone’s saliva. When people wore the testing strip for 8 hours, the strip turned blue in response to amylase, while testing strips that weren’t exposed to saliva stayed white.
What to Look For
When this project began, scientists were primarily focused on two main ways to detect COVID-19 — approaches that are still being used now, both at home and in the lab. One of these methods is the approach used in a COVID-19 PCR test: Find the virus by amplifying and looking for its genetic material in the form of RNA. The other approach is to look for COVID-19 antigens, proteins that are produced by the virus; this is what an at-home COVID-19 test screens for in a swab sample.
The researchers wondered whether there might be a more straightforward approach. “PCR uses thermal cycling to amplify the genetic material. Here, we wanted to use the natural enzymatic properties of SARS biomarkers for detection,” said Jokerst, whose work focuses on health-related imaging. They came up with proteases — enzymes that the virus uses to break apart proteins and which it needs to reproduce. These proteases are a good target because they are unique to a particular group of coronaviruses that cause SARS, MERS, and COVID-19 but are not found in humans.
A color-changing mask could quickly and easily act as a tool to monitor for both COVID-19 and future diseases, particularly for groups that may be more vulnerable to infectious diseases, Jokerst said.
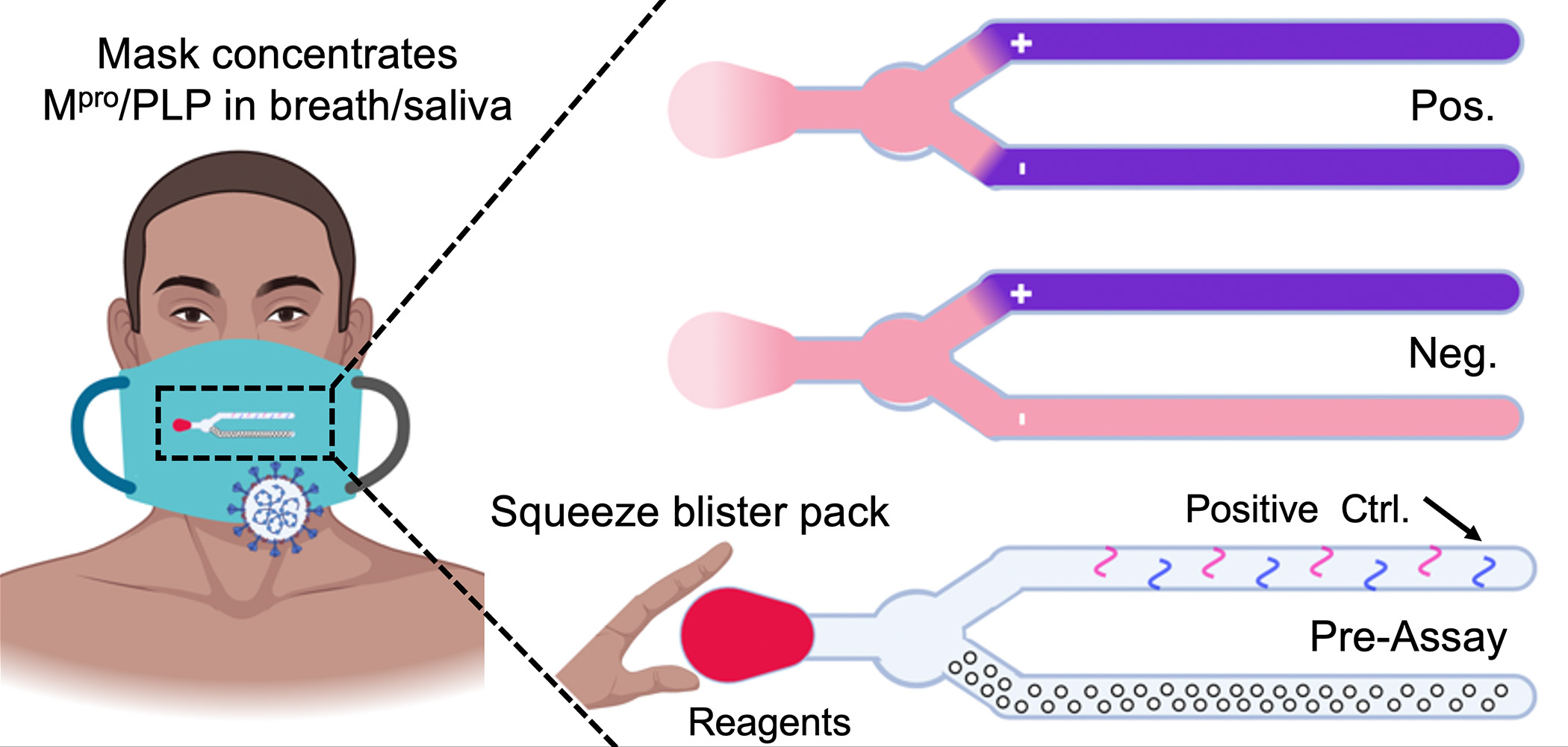
The smart mask would contain a sensor that monitors the presence of a SARS-CoV-2 protease in the breath. When the person wearing the mask breaks the blister pack, a chemical reaction takes place that causes the sensor to change color when the virus is detected. Image courtesy of Jesse Jokerst, Ph.D.
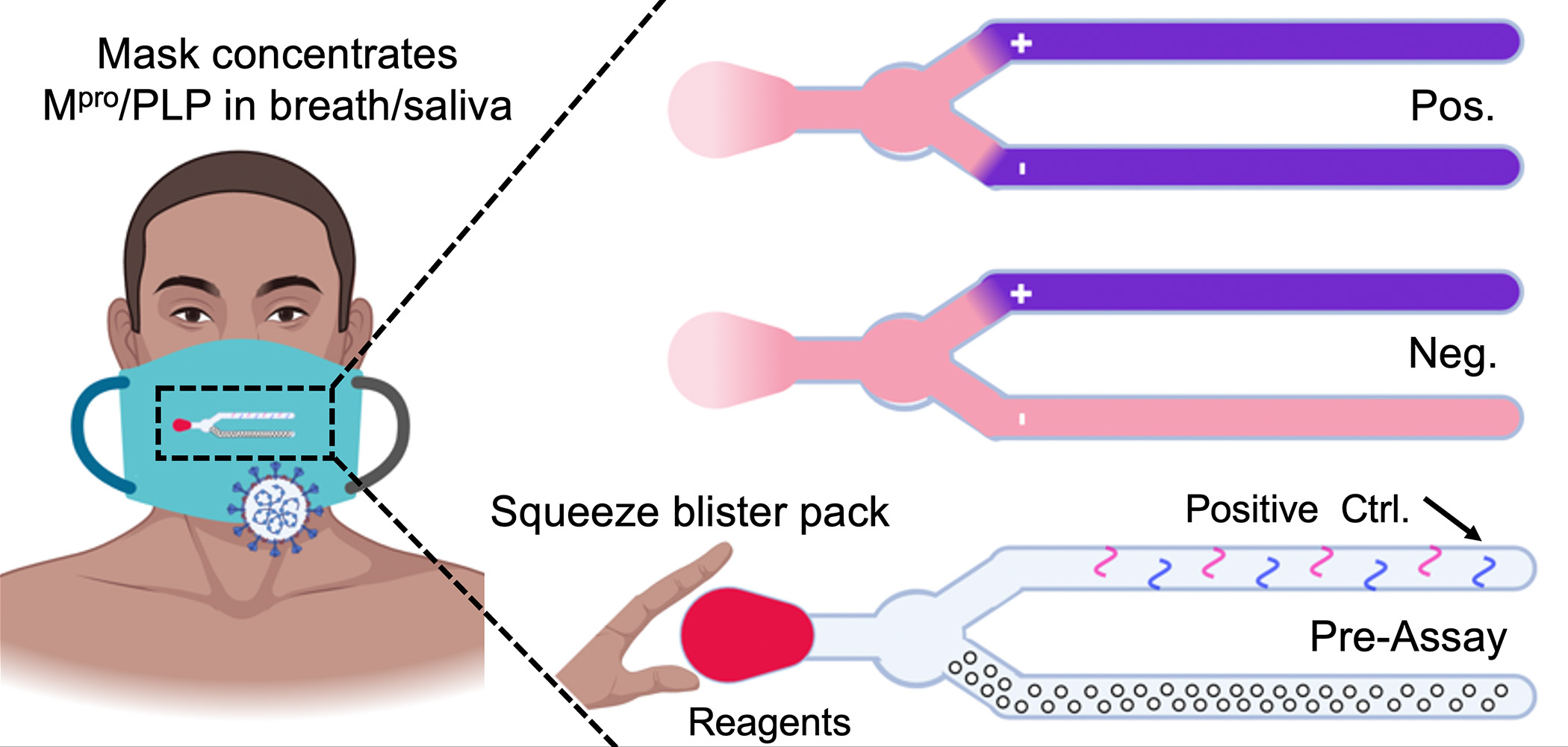
The smart mask would contain a sensor that monitors the presence of a SARS-CoV-2 protease in the breath. When the person wearing the mask breaks the blister pack, a chemical reaction takes place that causes the sensor to change color when the virus is detected. Image courtesy of Jesse Jokerst, Ph.D.
Color Change Is Easy, Detection Is Harder
The smart mask sensor has the benefit of simplicity. When a person breaks the blister-sealed pack, a reaction takes place — after about 10 minutes, if SARS-CoV-2 is present, the sensor strip turns blue. The sensor’s chemistry is quite stable, Jokerst said, so these masks would work easily wherever they could be worn, without concerns about storage or handling.
This ease of use, right on site, means that people invested in workplace safety were among the first to contact Jokerst when he and his team began discussing their project publicly. “In a warehouse, you bring a bunch of people together for 8 to 12 hours, then send them out into the world,” Jokerst said. Employers were interested in using smart masks to prevent or contain spreading events. The masks could also be used in other settings, such as travel or large events. “You wear this sticker, and it accumulates your breath over a workday or a flight to San Francisco,” he said. “At the end of that, you press the blister pack and the fluid releases,” indicating whether you have SARS-CoV-2 markers in your breath and need diagnostic testing, such as a PCR test.
One of the challenges this effort has faced is creating a smart mask that can recognize tiny amounts of the protease. When a person has COVID-19, the virus breaks into their body’s cells and takes over, using human cells to make more viruses. In order to reach the sensor, the cell has to die, the dead cell and its proteases have to get into the breath, and the breath needs to condense onto the sensor. This can and does happen; as well as harnessing cells to reproduce, SARS-CoV-2 is known to actively kill immune cells, and these dead cells make their way out of the body in fluids, including saliva. But getting enough of these cells is tricky, Jokerst said. “The detection limits that we’re pushing up against are very, very low.”

Developing a Smart Mask to Surveil Coronavirus
NIDCR reports on the successful feasibility testing of smart masks that are being developed to identify cases of COVID-19.
Future Directions
The results of Jokerst’s study are promising. So far, the team has tested more than 100 samples from people with COVID-19 using their current sensor and have had very few false positives — that is, the sensor almost never changed color when SARS-CoV-2 proteases were not present. The researchers are actively working to identify which of the dozens of coronavirus proteases will provide the best results.
The team is turning to smart mask technology to identify other pathogens as well, particularly fungal diseases. Although viruses replicate and use proteases inside the cell, Jokerst said, fungi that cause disease make their proteins outside of the infected cells, meaning that the detection of fungal proteases is much easier. Diseases caused by fungi include Valley fever and Pneumocystis pneumonia.
Once smart masks are fully functional, the benefit extends far beyond the current pandemic. The current PCR tests might need to be modified to look for genetic material from future viruses, and tests that scan for the coronavirus’ unique spike proteins might also need to be reinvented for other variants. But the smart masks search for proteases that are very likely to be produced by future coronaviruses. This team’s smart masks would be ready to go, Jokerst said. “Having this on the shelf would allow almost immediate detection.”
Sources
Jin, Z., Mantri, Y., Retout, M., Cheng, Y., Zhou, J., Jorns, A., Fajtova, P., Yim, W., Moore, C., Xu, M., Creyer, M. N., Borum, R. M., Zhou, J., Wu, Z., He, T., Penny, W. F., O’Donoghue, A. J., & Jokerst, J. V. (2022). A charge-switchable zwitterionic peptide for rapid detection of SARS-CoV-2 main protease. Angewandte Chemie International Edition, 61(9), e202112995. https://doi.org/10.1002/anie.202112995
Jin, Z., Jorns, A., Yim, W., Wing, R., Mantri, Y., Zhou, J., Zhou, J., Wu, Z., Moore, C., Penny, W. F., & Jokerst, J. V. (2021). Mapping aerosolized saliva on face coverings for biosensing applications. Analytical Chemistry, 93(31), 11025–11032. https://doi.org/10.1021/acs.analchem.1c02399
Retout, M., Mantri, Y., Jin, Z., Zhou, J., Noël, G., Donovan, B., Yim, W., & Jokerst, J. V. (2022). Peptide-induced fractal assembly of silver nanoparticles for visual detection of disease biomarkers. ACS Nano, 16(4), 6165–6175. https://doi.org/10.1021/acsnano.1c11643
 An official website of the United States government
An official website of the United States government


