Article Highlights
-
When multiple organs have failed due to COVID-19, many people never recover.
-
Washing the inside of the belly, or abdomen with fluid may help prevent organ failure.
-
A new device can wash the inside of the abdomen in the patient’s ICU bed without surgery.
The most common symptoms of COVID-19—such as cough, fever, and shortness of breath—relate to the respiratory system. But early in the pandemic, doctors began reporting that sometimes the damage went further.
“When COVID hit, it became clear to us that it had pretty devastating consequences on various organ systems,” said Daniel Burnett, M.D., the founder and CEO of TheraNova, a company in San Francisco that develops medical devices. “It can really have a dramatic impact on the lungs or the heart, liver, intestine, and kidneys.” Once multiple organs have failed, many people never recover.
Burnett and his colleagues realized they had something that could help: a device designed to support organ health for people in the intensive care unit (ICU). They applied for—and received—funding from the National Institute on Aging (NIA) to continue developing the device.
Washing the belly
The new invention delivers a treatment known as direct peritoneal resuscitation.
Direct peritoneal resuscitation washes the inside of the abdomen (the belly area) with water mixed with sugar, salt, and other additives. This is thought to support the organs in various ways. For example, it may take over the role of the kidneys by soaking up toxins from the blood. In fact, every day thousands of people with kidney failure use the same solution at home, putting fluid into the abdomen, then draining it in a treatment known as peritoneal dialysis. It’s an alternative to going to a center for hemodialysis, often just called dialysis.
Preliminary studies have found that direct peritoneal resuscitation can improve the health of failing organs. But getting the fluid into the belly requires implanting a catheter, which is normally done with surgery. A person who is on life support in the ICU is too sick for that. Burnett and his colleagues are developing a safer way to give the treatment.
“When COVID hit, it became clear to us that it had pretty devastating consequences on various organ systems.” —Daniel Burnett, M.D.
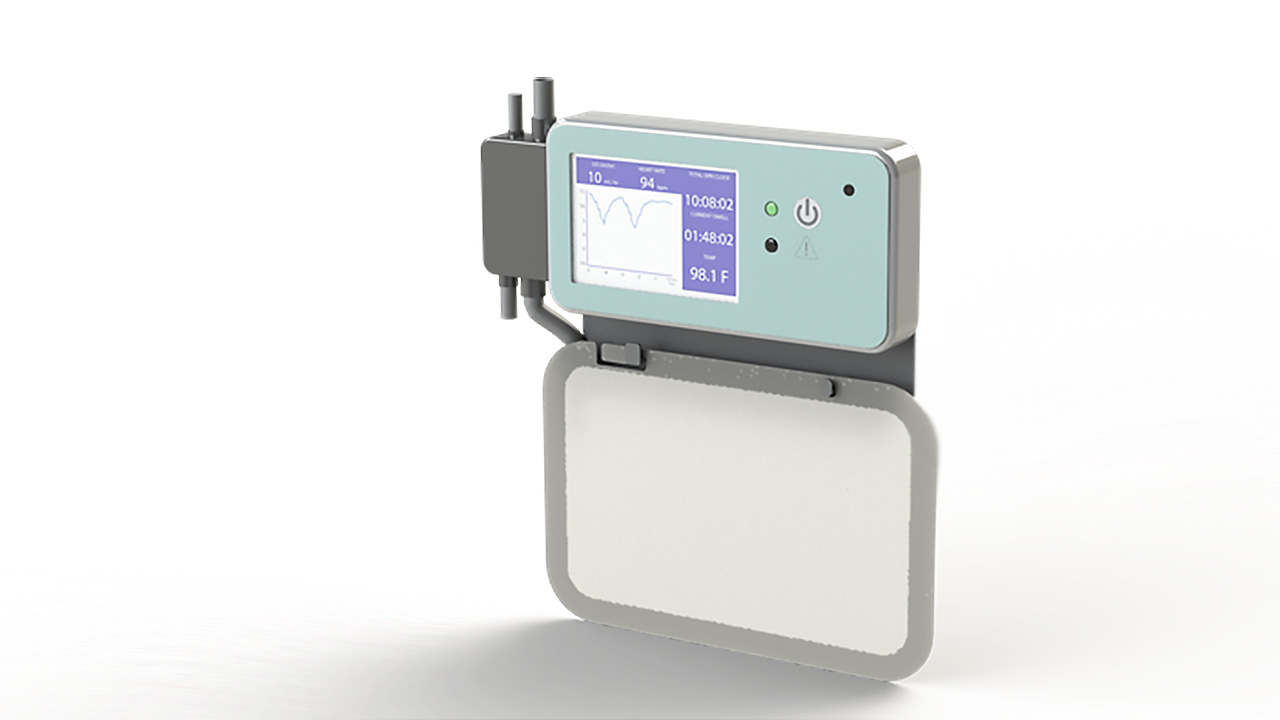
The fluid lavage controller is part of a medical device that TheraNova is developing to support organ health for people in the ICU. Photo: TheraNova
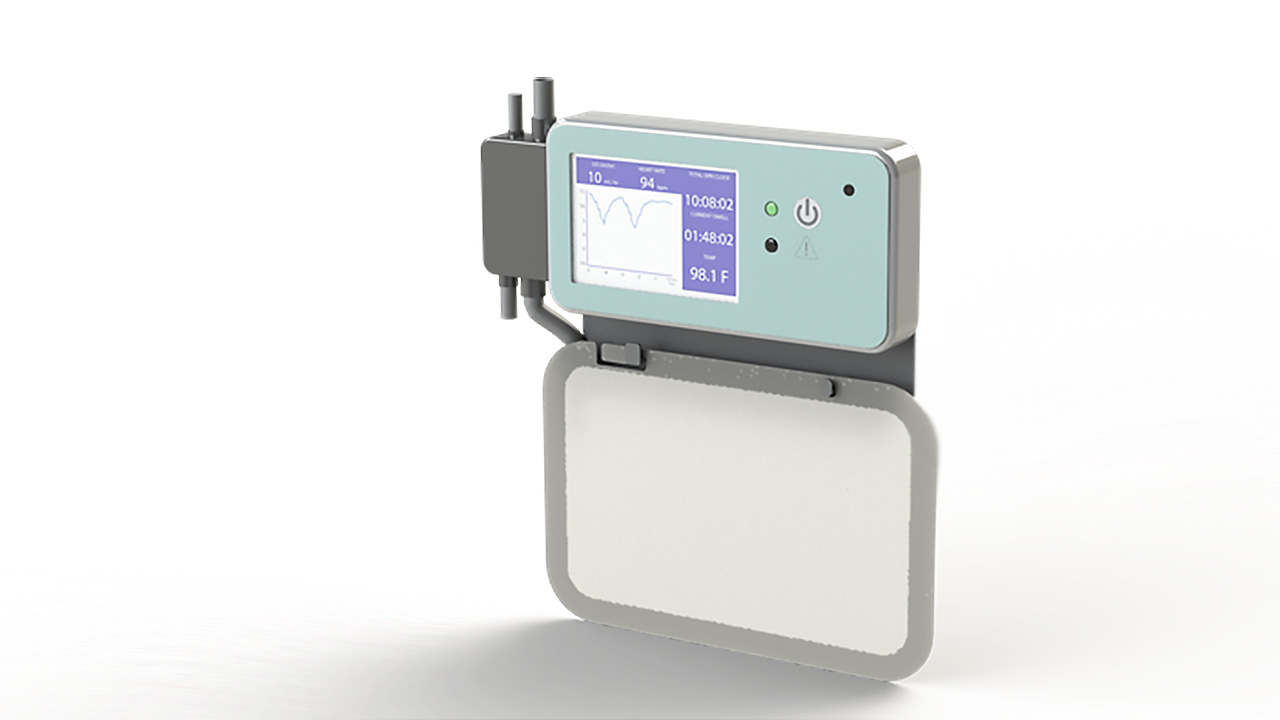
The fluid lavage controller is part of a medical device that TheraNova is developing to support organ health for people in the ICU. Photo: TheraNova
The new invention
The invention makes it possible to wash the inside of the belly without surgery. A doctor uses an access device to make a cut in the wall of the belly. This can be done at the patient’s bed in the ICU. Then the doctor inserts a special 18-inch-long catheter with a weighted tip and starts fluid flowing through. The fluid makes the catheter gently shake and wiggle its way around the organs. The weighted tip sinks through the person’s belly to settle behind the intestines.
The catheter has a sensor that measures the pressure inside the belly. A machine, known as the fluid lavage controller, at the bedside keeps the fluid flowing, making sure the pressure in the abdomen stays safe—pumping in too much liquid can compress the organs and cause serious problems.
Once the catheter is in place, it continuously circulates fluid through the belly. Clean fluid flows through an opening in the catheter positioned just inside the front of the belly. The fluid bathes the large and small intestines, spleen, and other organs in the abdomen. Then the fluid flows out through the tip of the catheter.
Scientists are not sure exactly how this fluid helps. It may take over some of the work that the organs are supposed to be doing, and it may also provide nutrition to the internal organs. But even with this uncertainty, enough experiments have shown that it might help to make it worth testing further, Burnett said.
Next steps
TheraNova was founded in 2005 as a medical device incubator. The company carries out the earliest stages of development for new devices. If a device has good results, TheraNova starts a new company to continue developing the invention.
Burnett and his team are finalizing their algorithm now and hope to start testing the invention in pigs this year. If preclinical tests are successful, TheraNova will start a new company to carry the invention forward, with testing in humans. Normally, it might take two or three years for the device to be approved for use by doctors, but if the invention is very promising and multiple organ failure in COVID-19 patients continues to be a significant problem, the device might be able to get to market faster.
“Our eventual hope is that anybody, anywhere, who is in critical care and is experiencing multiorgan failure can have this to help support their organs and, hopefully, bridge them to a good outcome,” Burnett said.
 An official website of the United States government
An official website of the United States government

