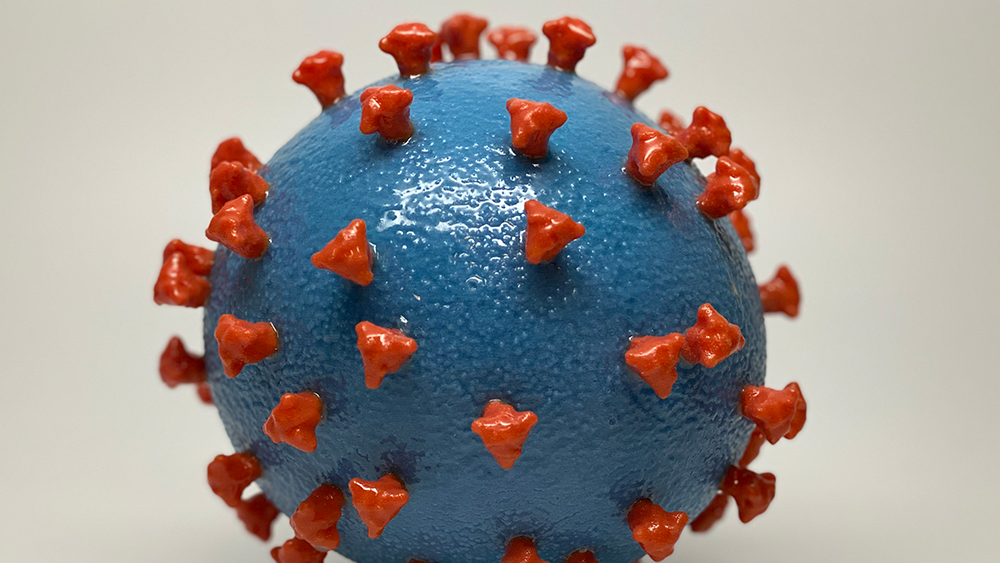
A 3D-printed model of SARS-CoV-2, the virus that causes COVID-19. Spike proteins (shown in red) stud the smooth surface of the virus (blue). The spike proteins enable the virus to infect human cells. Scientists are racing to develop vaccines that may protect against current and future variants that have mutated spike proteins. Image courtesy of NIH.
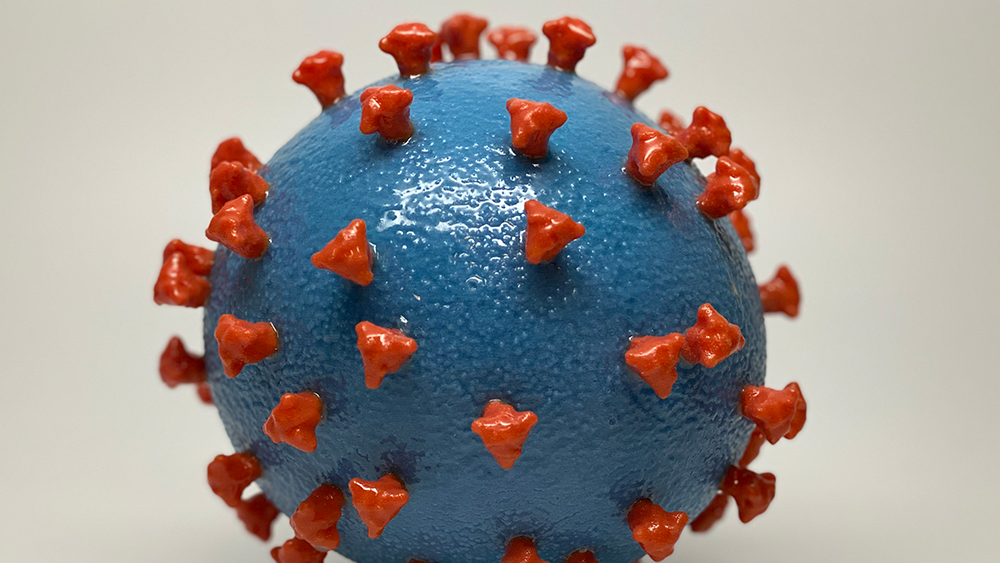
A 3D-printed model of SARS-CoV-2, the virus that causes COVID-19. Spike proteins (shown in red) stud the smooth surface of the virus (blue). The spike proteins enable the virus to infect human cells. Scientists are racing to develop vaccines that may protect against current and future variants that have mutated spike proteins. Image courtesy of NIH.
What you need to know
Since the spring of 2021, the majority of COVID-19 infections in the United States have been caused by variants of SARS-CoV-2. Variants emerge as the virus multiplies and its genetic material changes. These mutations can alter the spike proteins on the viral surface. If this happens, antibodies produced after COVID-19 vaccination or recovery from infection may not be able to stick to the virus. This raises the risk that SARS-CoV-2 variants can escape from antibodies that usually help prevent COVID-19.
The Omicron variant — the most common cause of COVID-19 in the United States since December 2021 — has almost 50 mutations in its spike protein. The changes make it easier for the virus to spread, and although existing vaccines do provide good protection against severe COVID-19 caused by Omicron and current variants, the changes limit the vaccines’ effectiveness.
Scientists are working on new types of vaccines to combat current and future SARS-CoV-2 variants. A study supported by the National Institute of Allergy and Infectious Diseases (NIAID) showed that two experimental vaccines protected mice against SARS-CoV-2 by activating immune cells in the airways and lungs rather than relying on antibodies.
What did the researchers do?
The researchers developed two vaccines that work in a different way than currently approved COVID-19 vaccines, which target parts of the spike protein that often change. The experimental vaccines target parts of the spike protein that rarely mutate. The vaccines also boost the activity of immune cells called mucosal T cells that live in the respiratory system.
The team vaccinated the mice and, 3 to 5 months later, exposed them to either the original strain of SARS-CoV-2 or the Beta variant. The activated mucosal T cells destroyed cells infected with SARS-CoV-2. The vaccinated mice had very little virus in their lungs compared with unvaccinated mice and were protected from severe illness. This protection did not depend on antibodies produced in response to the vaccines.
The results suggest that these vaccines might prevent severe COVID-19 caused by any variant. The researchers believe it may be possible to create a vaccine that not only activates mucosal T cells but also stimulates production of antibodies and immune cells aimed at the spike protein. This double strategy might be the best way to protect against COVID-19 caused by current or future variants.
Why is this research important?
As long as SARS-CoV-2 continues to spread, new variants can evolve. The promising results of this basic research suggest that activating mucosal T cells may be a way to fight COVID-19 regardless of which strain of SARS-CoV-2 is on the rise.
In the meantime, everyone can play a role in preventing the emergence of dangerous SARS-CoV-2 variants. Full vaccination, including booster doses, continues to provide good protection against severe COVID-19, even if caused by variants, including Omicron.
Where can I go to learn more?
T cells protect against COVID-19 in absence of antibody response
-
An article in NIH Research Matters explains the results of tests of the experimental vaccines in mice.
-
The Centers for Disease Control and Prevention (CDC) provides information about variants, including a video explaining how CDC scientists track the virus’s genetic changes.
Coronavirus Vaccines and Prevention
-
NIAID explains research on vaccines to prevent COVID-19 and other diseases caused by coronaviruses.
Sources
Centers for Disease Control and Prevention. (2022). What you need to know about variants. Accessed June 22, 2022, from https://www.cdc.gov/coronavirus/2019-ncov/variants/about-variants.html.
Hong, Q., Han, W., Li, J., Xu, S., Wang, Y., Xu, C., Li, Z., Wang, Y., Zhang, C., Huang, Z., & Cong, Y. (2022). Molecular basis of receptor binding and antibody neutralization of Omicron. Nature, 604(7906), 546-552. https://doi.org/10.1038/s41586-022-04581-9
Johnson, A. G., Amin, A. B., Ali, A. R., Hoots, B., Cadwell, B. L., Arora, S., Avoundjian, T., Awofeso, A. O., Barnes, J., Bayoumi, N. S., Busen, K., Chang, C., Cima, M., Crockett, M., Cronquist, A., Davidson, S., Davis, E., Delgadillo, J., Dorabawila, V., Drenzek, C., … Scobie, H. M. (2022). COVID-19 incidence and death rates among unvaccinated and fully vaccinated adults with and without booster doses during periods of Delta and Omicron variant emergence — 25 U.S. jurisdictions, April 4-December 25, 2021. Morbidity and Mortality Weekly Report, 71(4), 132-138. https://doi.org/10.15585/mmwr.mm7104e2
Kingstad-Bakke, B., Lee, W., Chandrasekar, S. S., Gasper, D. J., Salas-Quinchucua, C., Cleven, T., Sullivan, J. A., Talaat, A., Osorio, J. E., & Suresh, M. (2022). Vaccine-induced systemic and mucosal T cell immunity to SARS-CoV-2 viral variants. Proceedings of the National Academy of Sciences of the United States of America, 119(20), e2118312119. https://doi.org/10.1073/pnas.2118312119

News and Stories
Read stories about the efforts underway to prevent, detect, and treat COVID-19 and its effects on our health.
 An official website of the United States government
An official website of the United States government

