On This Page:


Understanding COVID-19 Vaccines
Which COVID-19 vaccines are available in the United States?
On September 11, 2023, the U.S. Food and Drug Administration (FDA) updated the emergency use authorizations for two mRNA COVID-19 vaccines. The updated vaccines are composed of a formula that provides extra protection against currently circulating variants. Both vaccines are authorized for anyone who is at least six months old.
-
Moderna COVID-19 Vaccine, 2023-2024 Formula: This vaccine is an updated version of the NIH-funded, FDA-approved mRNA-1273 vaccine (Spikevax) that has more activity against the Omicron XBB.1.5 strain View the infographic to see what is in the original Moderna COVID-19 vaccine.
-
Pfizer, Inc., and BioNTech COVID-19 Vaccine, 2023-2024 Formula: This vaccine is an updated version of the FDA-approved BNT162b2 vaccine (Comirnaty) that has more activity against the Omicron XBB.1.5 strain. View the infographic to see what is in the original Pfizer COVID-19 vaccine.
Two other COVID-19 vaccines have been authorized for certain groups.
-
Novavax COVID-19 Vaccine, Adjuvanted: On July 13, 2022, the FDA reauthorized emergency use of this two-dose vaccine series for people age 12 and older. This is the first protein-based COVID-19 vaccine to receive FDA authorization and is similar in design to vaccines against the flu and shingles. The FDA has also authorized Novavax as a booster vaccination for people age 18 and older who cannot access other COVID-19 vaccines, people for whom other COVID-19 vaccines are not clinically appropriate, or people who would not otherwise receive a COVID-19 vaccine.
-
Janssen Pharmaceutical Companies of Johnson & Johnson: On March 13, 2023, the FDA reauthorized emergency use of this vaccine for use in people 18 and older who cannot access other COVID-19 vaccines, people for whom other COVID-19 vaccines are not clinically appropriate, or people who would not otherwise receive a COVID-19 vaccine.
Do I need an updated COVID-19 vaccine?
Protection against SARS-CoV-2 begins to decrease over time after a person’s first vaccine doses — the primary vaccine series. For the best protection from COVID-19, the Centers for Disease Control and Prevention (CDC) recommends that everyone 6 months and older stay up to date on their COVID-19 vaccines, including getting updated vaccine doses if eligible.
Updated versions of COVID-19 vaccines may be authorized each year to provide extra protection against new, common viral variants. People who are 65 or older or who are immunocompromised may need more booster doses.
Can children get a vaccine?
Children and teens age 6 months and older can get the updated Pfizer and Moderna COVID-19 vaccines, and children and teens age 12 and older can get the Novavax COVID-19 vaccine.
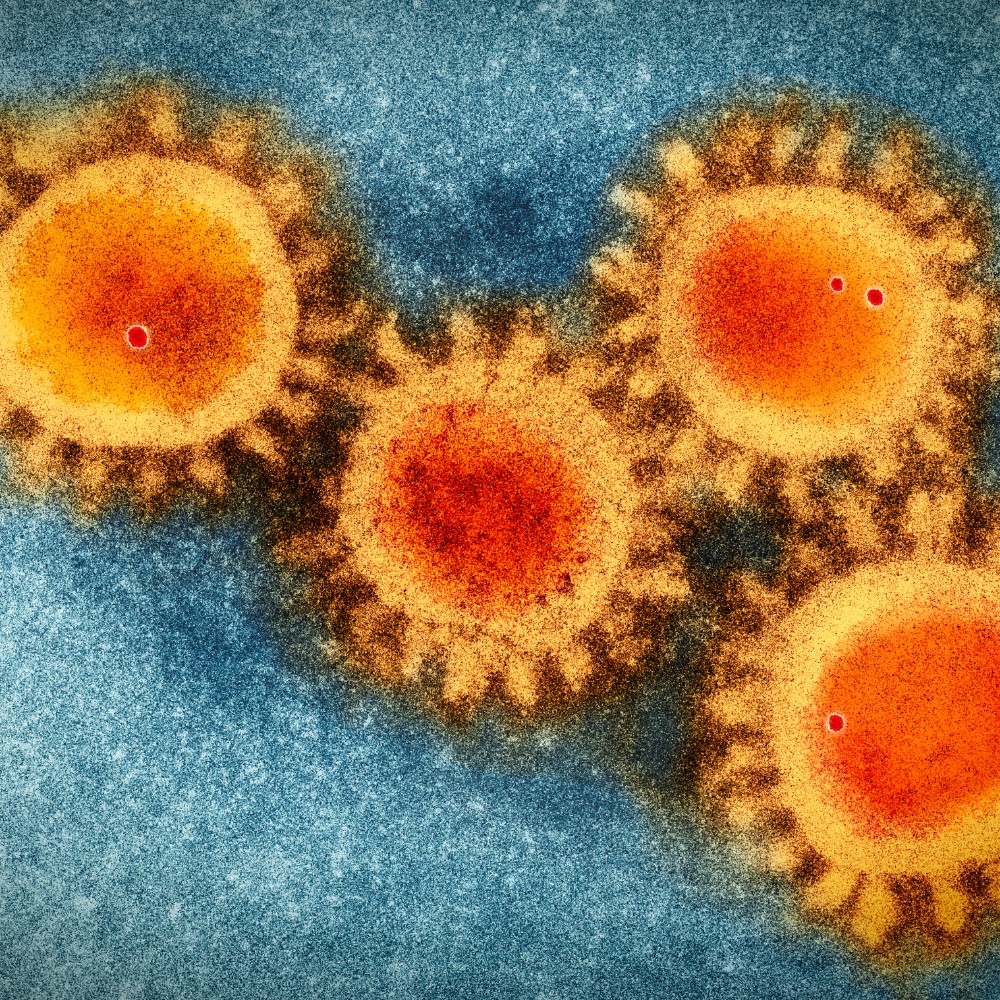
Do the vaccines protect against virus variants?
Studies and current data show that the antibodies our bodies make after vaccination recognize and protect against COVID-19 variants like Omicron. However, studies also show that the protection against variants offered by the original COVID-19 vaccines wanes substantially over time. The updated mRNA vaccines offer increased protection against SARS-CoV-2 infection and severe COVID-19.
Do the vaccines work?
Studies show that COVID-19 vaccines are very effective in preventing COVID-19, even for people at high risk for the disease. By the end of November 2021, scientists estimate that mRNA COVID-19 vaccines had prevented at least 1 million deaths, 10 million hospitalizations, and 36 million SARS-CoV-2 infections in the United States.
Sometimes people who are fully vaccinated get a breakthrough infection, meaning that they test positive for SARS-CoV-2 or become ill with COVID-19. Fully vaccinated people are less likely to become seriously ill, even from COVID-19 variants.
How do I know the vaccines are safe?
Vaccines have very high safety standards, and COVID-19 vaccines are no exception. COVID-19 vaccines have undergone and will continue to undergo the most intensive safety monitoring in U.S. history.
The timeline for creating COVID-19 vaccines was shorter than for other vaccines for many reasons, including the following:
-
NIH scientists have been studying mRNA vaccines and coronaviruses for decades. Scientists had a head start because they already knew a lot about how mRNA vaccines work and how to make them.
-
Researchers, the federal government, and drug companies came together like never before to cooperate and share resources, making the vaccine testing process more efficient.
-
NIH set up the COVID-19 Prevention Network (CoVPN) to coordinate existing research networks and carry out large clinical trials in tens of thousands of people efficiently. Many Americans from diverse communities volunteered to participate in the studies.
-
The FDA analyzed data from the clinical trials right away.
The safety of the authorized COVID-19 vaccines is being tracked through the Vaccine Adverse Event Reporting System (VAERS), a unique safety system called v-safe that was established specifically for COVID-19 vaccines, and other systems. Vaccine manufacturers submit monthly safety updates to the FDA. The FDA also inspects vaccine production facilities and checks the quality of vaccine batches.
Do the vaccines have any side effects?
All vaccines may cause some side effects, which are normal signs that your body is making antibodies. These side effects go away in a few days. Many people have no side effects.
Serious side effects that could cause long-term health problems are extremely unlikely after any vaccination, including COVID-19 vaccination. These rare side effects usually appear within six weeks of receiving a vaccine dose. If you have health problems after vaccination, talk to your health care provider and report the problem to VAERS.
Rare cases of heart inflammation have been reported after mRNA COVID-19 vaccination, mainly in male adolescents and young adults.
CDC continues to recommend vaccination for everyone 6 months of age and older, given the greater risk of serious complications related to COVID-19.
How COVID-19 Affects Pregnancy
Should you get the vaccine during pregnancy? Does the vaccine cause infertility? NIH research is helping to answer these questions and more.


How do I get a COVID-19 vaccine?
The federal government is providing FDA-authorized and approved COVID-19 vaccines free to all people living in the United States, regardless of their immigration or health insurance status.
Search Vaccines.gov, text your ZIP code to 438829, or call 1-800-232-0233 to find COVID-19 vaccine locations near you. Contact your state health department to find additional vaccination locations in your area.
If you have difficulty reaching a vaccination site, you may be able to get an in-home vaccination. Check a list of services that may offer in-home COVID-19 vaccinations in your area.
Should I get a vaccine if I've had COVID-19 in the past?
Studies indicate that vaccination produces a stronger immune response than the one produced by COVID-19 infection. The benefits of vaccination after infection far outweigh any known or potential risks.
To ensure that people who recover from COVID-19 are protected from getting the disease again, CDC recommends that they get vaccinated. The timing of vaccination depends on when a person had COVID-19 and whether and when they received treatment. If you have had COVID-19 and want to be vaccinated, talk to your doctor about when you should get the vaccine.
Are there any circumstances under which I should not get vaccinated?
Vaccination is recommended for everyone who is eligible. If you have a medical condition and are concerned about how COVID-19 vaccination may affect you, talk to your health care provider about whether getting vaccinated is right for you.
Due to safety concerns, CDC recommends that the Johnson & Johnson/Janssen COVID-19 vaccines only be considered in certain situations.
Are vaccines still being researched?
New and ongoing studies on vaccines are underway. NIH Institutes and Centers, in partnership with private businesses and other federal agencies, continue to study COVID-19 vaccines and strategies to encourage vaccination within vulnerable communities.
Many current studies are monitoring the health of vaccinated people to determine the vaccines' effectiveness over a longer period of time. Other research aims to develop new vaccines that might protect against current and future types of coronaviruses.
The Journey of a Vaccine
Learn about the four phases of clinical research, what questions researchers try to answer in each, and how a vaccine is developed, approved, and manufactured.
COVID-19 Vaccine Resources
HHS shares information about the vaccine distribution process.
Get the facts about COVID-19 vaccine studies.
NIH and other federal agencies sponsor vaccine trials that are seeking research volunteers.
CDC shares answers to some common questions about COVID-19 vaccines.
 An official website of the United States government
An official website of the United States government